03 Aug Know your Diabetes
What is diabetes
Diabetes is a chronic disease that occurs when the pancreas is no longer able to make insulin, or when the body cannot make good use of the insulin it produces.
Insulin is a hormone made by the pancreas, that acts like a key to let glucose from the food we eat pass from the blood stream into the cells in the body to produce energy. All carbohydrate foods are broken down into glucose in the blood. Insulin helps glucose get into the cells.
Not being able to produce insulin or use it effectively leads to raised glucose levels in the blood (known as hyperglycaemia). Over the long-term high glucose levels are associated with damage to the body and failure of various organs and tissues.
Types of diabetes
Top of Form
There are three main types of diabetes:
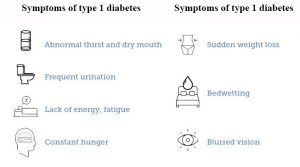
Type 1 diabetes used to be called juvenile-onset diabetes. It is usually caused by an auto-immune reaction where the body’s defence system attacks the cells that produce insulin. The reason this occurs is not fully understood. People with type 1 diabetes produce very little or no insulin. The disease may affect people of any age, but usually develops in children or young adults. People with this form of diabetes need injections of insulin every day in order to control the levels of glucose in their blood. If people with type 1 diabetes do not have access to insulin, they will die.
Type 2 diabetes used to be called non-insulin dependent diabetes or adult-onset diabetes, and accounts for at least 90% of all cases of diabetes. It is characterised by insulin resistance and relative insulin deficiency, either or both of which may be present at the time diabetes is diagnosed. The diagnosis of type 2 diabetes can occur at any age. Type 2 diabetes may remain undetected for many years and the diagnosis is often made when a complication appears or a routine blood or urine glucose test is done. It is often, but not always, associated with overweight or obesity, which itself can cause insulin resistance and lead to high blood glucose levels. People with type 2 diabetes can often initially manage their condition through exercise and diet. However, over time most people will require oral drugs and or insulin.
Both type 1 and type 2 diabetes are serious. There is no such thing as mild diabetes.
Gestational diabetes (GDM) is a form of diabetes consisting of high blood glucose levels during pregnancy. It develops in one in 25 pregnancies worldwide and is associated with complications to both mother and baby. GDM usually disappears after pregnancy but women with GDM and their children are at an increased risk of developing type 2 diabetes later in life. Approximately half of women with a history of GDM go on to develop type 2 diabetes within five to ten years after delivery.
Other specific types of diabetes also exist.
Diabetes risk factors
The risk factors for type 1 diabetes are still being researched. However, having a family member with type 1 diabetes slightly increases the risk of developing the disease. Environmental factors and exposure to some viral infections have also been linked to the risk of developing type 1 diabetes.
Several risk factors have been associated with type 2 diabetes and include:
- Family history of diabetes
- Overweight
- Unhealthy diet
- Physical inactivity
- Increasing age
- High blood pressure
- Ethnicity
- Impaired glucose tolerance (IGT)*
- History of gestational diabetes
- Poor nutrition during pregnancy
*Impaired glucose tolerance (IGT) is a category of higher than normal blood glucose, but below the threshold for diagnosing diabetes.
Changes in diet and physical activity related to rapid development and urbanisation have led to sharp increases in the numbers of people developing diabetes.
Pregnant women who are overweight, have been diagnosed with IGT, or have a family history of diabetes are all at increased risk of developing gestational diabetes mellitus (GDM). In addition, having been previously diagnosed with gestational diabetes or being of certain ethnic groups puts women at increased risk of developing GDM.

Diabetes complications
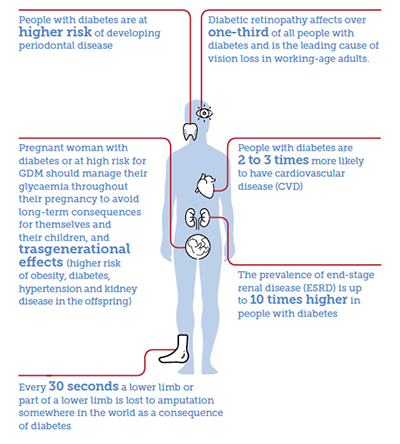
People with diabetes have an increased risk of developing a number of serious health problems. Consistently high blood glucose levels can lead to serious diseases affecting the heart and blood vessels, eyes, kidneys, nerves and teeth. In addition, people with diabetes also have a higher risk of developing infections. In almost all high-income countries, diabetes is a leading cause of cardiovascular disease, blindness, kidney failure, and lower limb amputation.
Maintaining blood glucose levels, blood pressure, and cholesterol at or close to normal can help delay or prevent diabetes complications. Therefore people with diabetes need regular monitoring.
Cardiovascular disease: affects the heart and blood vessels and may cause fatal complications such as coronary artery disease (leading to heart attack) and stroke. Cardiovascular disease is the most common cause of death in people with diabetes. High blood pressure, high cholesterol, high blood glucose and other risk factors contribute to increasing the risk of cardiovascular complications.
Kidney disease (diabetic nephropathy): caused by damage to small blood vessels in the kidneys leading to the kidneys becoming less efficient or to fail altogether. Kidney disease is much more common in people with diabetes than in those without diabetes. Maintaining near normal levels of blood glucose and blood pressure can greatly reduce the risk of kidney disease.
Nerve disease (diabetic neuropathy): diabetes can cause damage to the nerves throughout the body when blood glucose and blood pressure are too high. This can lead to problems with digestion, erectile dysfunction, and many other functions. Among the most commonly affected areas are the extremities, in particular the feet. Nerve damage in these areas is called peripheral neuropathy, and can lead to pain, tingling, and loss of feeling. Loss of feeling is particularly important because it can allow injuries to go unnoticed, leading to serious infections and possible amputations. People with diabetes carry a risk of amputation that may be more than 25 times greater than that of people without diabetes. However, with comprehensive management, a large proportion of amputations related to diabetes can be prevented. Even when amputation takes place, the remaining leg and the person’s life can be saved by good follow-up care from a multidisciplinary foot team. People with diabetes should regularly examine their feet.
Eye disease (diabetic retinopathy): most people with diabetes will develop some form of eye disease (retinopathy) causing reduced vision or blindness. Consistently high levels of blood glucose, together with high blood pressure and high cholesterol, are the main causes of retinopathy. It can be managed through regular eye checks and keeping glucose and lipid levels at or close to normal.
Pregnancy complications: Women with any type of diabetes during pregnancy risk a number of complications if they do not carefully monitor and manage their condition. To prevent possible organ damage to the fetus, women with type 1 diabetes or type 2 diabetes should achieve target glucose levels before conception. All women with diabetes during pregnancy, type 1, type 2 or gestational should strive for target blood glucose levels throughout to minimize complications. High blood glucose during pregnancy can lead to the foetus putting on excess weight. This can lead to problems in delivery, trauma to the child and mother, and a sudden drop in blood glucose for the child after birth. Children who are exposed for a long time to high blood glucose in the womb are at higher risk of developing diabetes in the future.
Diabetes prevention
At present, type 1 diabetes cannot be prevented. The environmental triggers that are thought to generate the process that results in the destruction of the body’s insulin-producing cells are still under investigation.
While there are a number of factors that influence the development of type 2 diabetes, it is evident that the most influential are lifestyle behaviours commonly associated with urbanization. These include consumption of unhealthy foods and inactive lifestyles with sedentary behaviour. Randomised controlled trials from different parts of the world, including Finland, USA, China and India, have established the that lifestyle modification with physical activity and/or healthy diet can delay or prevent the onset of type 2 diabetes.
Modern lifestyles are characterised by physical inactivity and long sedentary periods. Community-based interventions can reach individuals and families through campaigns, education, social marketing and encourage physical activity both inside and outside school and the workplace. IDF recommends physical activity at least between three to five days a week, for a minimum of 30-45 minutes.
Taking a life course perspective is essential for preventing type 2 diabetes and its complications. Early in life, when eating and physical activity habits are established and when the long-term regulation of energy balance may be programmed, there is an especially critical window to prevent the development of overweight and reduce the risk of type 2 diabetes. Healthy lifestyles can improve health outcomes at later stages of life as well.
Population based interventions and policies allow healthy choices through policies in trade, agriculture, transport and urban planning to become more accessible and easy. Healthy choices can be promoted in specific settings (school, workplace and home) and contribute to better health for everyone. They include exercising regularly and eating wisely which will help to maintain normal levels of blood glucose, blood pressure and lipids.



